My husband takes carbidopa, I learned about carbidopa in medical school, but I haven't ever felt the need to dig too deeply into the mechanisms underlying carbadopa’s effects… until a few days ago when I was given the following article:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4211847/
The title alone made me skeptical — “The Parkinson’s disease death rate: carbidopa and vitamin B6.” Published in a relatively obscure journal, by individuals from non-academic institutions (not necessarily bad, but not the norm), I wanted to see what their claims were based on. So I read… and boy did they throw around scientific jargon. The article is not one that presents data to support claims. Instead, it’s a review/opinion piece. Typically, reviews are a great place to learn about a field. But here… my Scooby-senses told me that each “fact” may or may not be true. Perhaps because I’ve seen my own papers mis-cited, or perhaps because there were so many claims worded in absolutes (which you almost never see from true scientists), I decided to dig.
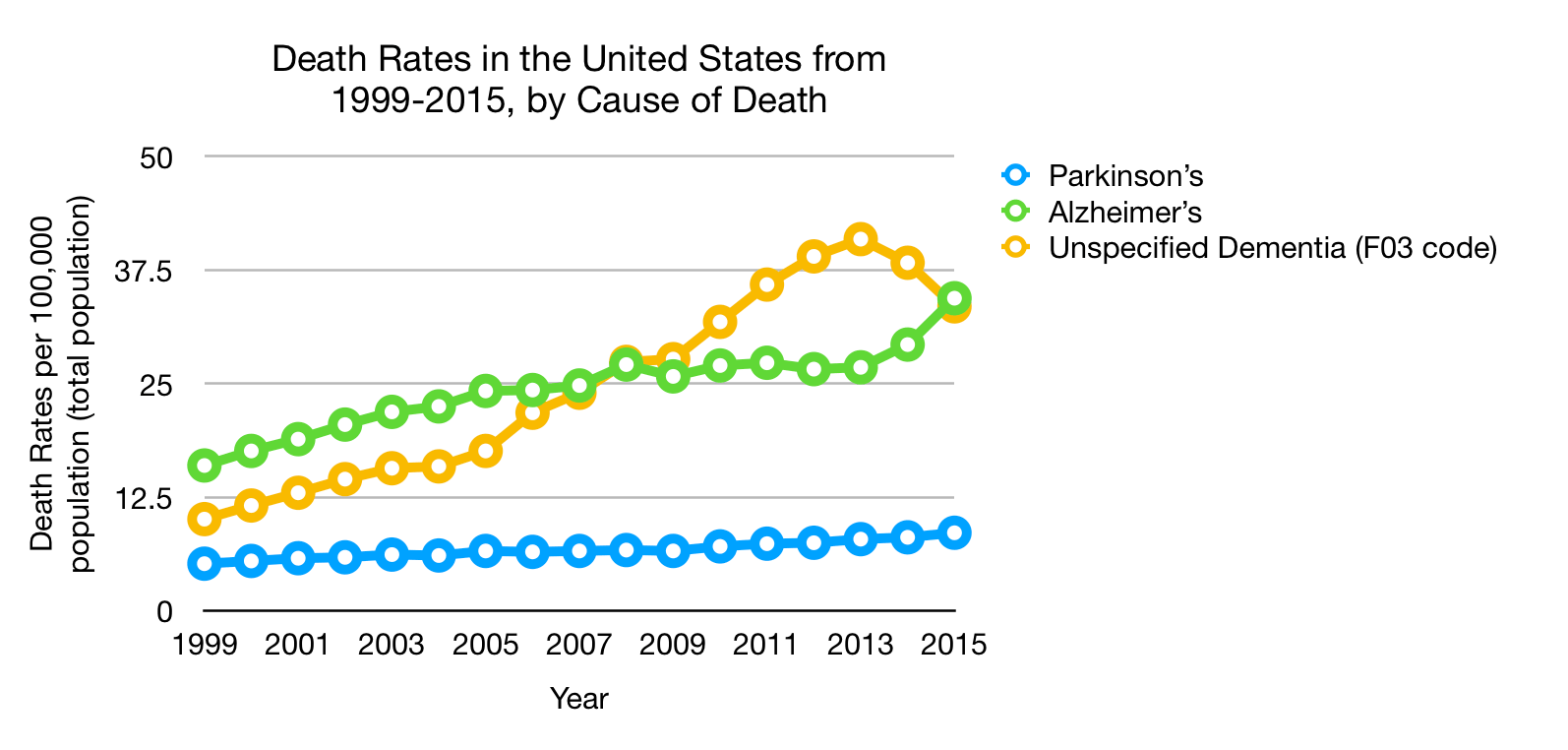
First off, that death-rate graph. What better way to stir up fear? When I look at the graph, one thing which immediately jumped out to me was a relatively linear increase in the death rate. The idea that a medication introduced in 1975 is continuing to cause a linear increase in the death rate seems strange to me. First off, according to the paper, L-dopa-only treatment no longer became available in 1999, and, now, 89% of people with Parkinson’s take carbidopa/L-dopa daily. If the effect were due to carbidopa, wouldn’t you expect the rate to have plateaued? I would. But, there are obviously other issues at play. First off, the data is based on the documented cause of death. Well, what if someone would have died from lung cancer had they gotten it in 1975, but improved treatments changed that outcome? What about the total number of people with PD (remember, these graphs are per 100,000 of the U.S. population as a whole)? Did they properly normalize the data for “white males 65 years and older, age-adjusted”? The list could go on and on. The number that I care about more is how long people are living with PD and their quality of life. Correlations are easy to make, causation is hard to prove. Using data from the U.S. Centers for Disease Control and Prevention (https://wonder.cdc.gov), I made the following graphs, which paint mortality due to PD in a slightly different picture.
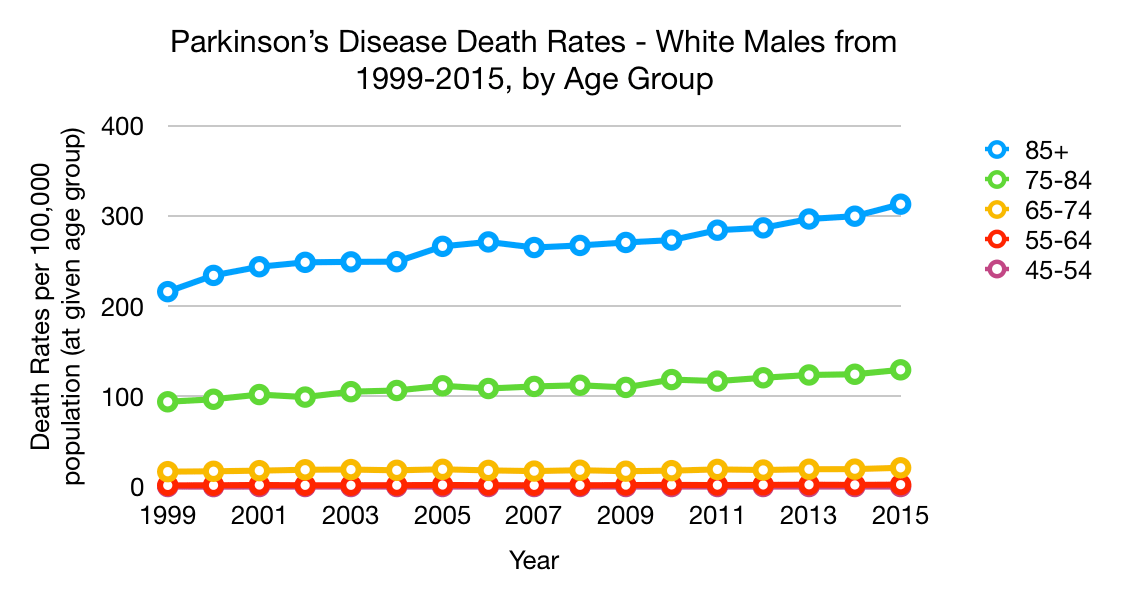
 Note, I did NOT adjust for age. In the second graph, the rates are using the population (and thus age demographics) of the given year. So in 2015, there were 1.9 million white males 85 or older and 6054 deaths, giving you a rate of 313 per 100,000 individuals 85+. As of now, I'm not entirely sure how Hinz and his colleagues were able to come up with their data for “white males 65 years and older, age adjusted." It’s not clear what data they normalized to, but my guess is they used population demographics from 1980 or 1990. In any case, the way they presented mortality data is incredibly skewed.
Note, I did NOT adjust for age. In the second graph, the rates are using the population (and thus age demographics) of the given year. So in 2015, there were 1.9 million white males 85 or older and 6054 deaths, giving you a rate of 313 per 100,000 individuals 85+. As of now, I'm not entirely sure how Hinz and his colleagues were able to come up with their data for “white males 65 years and older, age adjusted." It’s not clear what data they normalized to, but my guess is they used population demographics from 1980 or 1990. In any case, the way they presented mortality data is incredibly skewed.
Okay, now that we’ve look at the most frightening piece of data (and really the only piece of data presented in this paper), let’s look at the science they cited. Before I state my conclusions, I thought I’d walk you through what I did, some lines from the paper, and what I found from the references they used.
But first, let’s review the basics of what you need to know to follow my discussion. The main thing which comes up is PLP. What is it? It’s the active form of Vitamin B6 and acts as a co-factor for a lot of enzymes. As you may recall, enzymes are catalysts, so a cofactor is needed to catalyze specific reactions. You can essentially think B6 in place of PLP whenever I bring up PLP.
Diving right in with a quote from the paper:
“It [carbidopa] irreversibly binds to and permanently deactivates free PLP and PLP-dependent enzymes while inducing PLP reserve pool depletion.”
Is that true? The citation given is to the following paper, which is about finding a more selective inhibitor of DDC (the enzyme converting L-dopa to dopamine) than carbidopa — https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3285636/
In the introduction to this paper, the authors wrote “because hydrazine derivatives can react with free PLP and PLP-enzymes, these inhibitors are not entirely selective for DDC, thus resulting in adverse side effects.” Okay, they aren’t entirely selective… but how selective are they? By selectivity, I mean if the enzyme DCC were exposed to carbidopa and other enzymes were also exposed to carbidopa, how much of the carbidopa would be bound to DCC compared to the other enzymes? That is an answer that I have been unable to find. In their discussion, they go on to add “These adverse effects [side-effects from L-dopa with carbidopa and trihydroxybenzylhidrazine] can be ascribed, at least partially, to the mode of action of carbidopa and trihydroxybenzylhidrazine (the in vivo hydrolysis product of benserazide) that, by reacting non-enzymatically with free PLP, would cause PLP depletion” followed by “in addition, it must be pointed out that PD patients treated with L-Dopa and DDC peripheral inhibitors show high levels of plasmatic homocysteine.” You’ll notice that the authors of this other paper were careful in their wording.
Okay, that’s a start, but not incredibly helpful. So I looked at how carbidopa actually inhibits DCC. The crystal structure was published in 2001 in Nature Structural Biology — https://www.ncbi.nlm.nih.gov/pubmed/11685243. Essentially, carbidopa has multiple interactions, both with PLP (a co-factor) and with the enzyme itself. My take-away? Carbidopa does not bind solely to PLP to cause inhibition; there is at least some level of selectivity based on the interactions with the enzyme itself. I will say, my initial reading of the Hinz paper led me to believe that the way carbidopa was working was through binding only to PLP, which is not correct.
So what about carbidopa depleting PLP? After all, Hinz et al. stated: “Documentation submitted in 1997 noted significant central and peripheral PLP depletion after limited ingestion time of carbidopa.” Okay, let’s look at what that data is.
I took a look at the source they cited: http://www.metabolismjournal.com/article/0026-0495(78)90211-1/pdf Figure 2 in this paper nicely shows the levels of PLP in various tissues after administering carbidopa with or without pyridoxine 3x daily for 3 days to mice. But, the mice were given 10 or 100 mg/kg… for a 70 kg human (154 pounds), the dose would be 700-7000 mg 3x per day. Remember, clinical dosing of carbidopa is 10-25mg per pill. With the lower dose (10mg/kg), the effects of carbidopa administration were minimal on PLP levels in brain, hypothalamus, muscle, and liver. Serum showed decrease of ~70% from the lower (10 mg/kg) dose, and ~90% from the higher (100 mg/kg) dose. What does that mean? Well, there’s a dose effect… and we don’t have data for doses in the range of what is prescribed… that doesn’t mean there may not be an effect, but the idea that most people are completely ignoring research (as implied in the Hinz paper) or that giving mice the human equivalent of 21 grams of carbidopa (3x 7000mg) as proof of an effect is dubious. To give you an idea of the amount of just how much 21 grams of a drug is, a pill of (normal-dose) ibuprofen often contains 200 mg of the drug. To reach 21 grams per day, you would need to take 105 pills per day. A dose that high of ibuprofen would be fatal.
You may have noticed earlier that I quoted the following: “In addition, it must be pointed out that PD patients treated with L-Dopa and DDC peripheral inhibitors show high levels of plasmatic homocysteine.” (Daidone et al., 2012) I’ve heard that before, but what struck me was this line from the Hinz paper: “Parkinson’s disease is associated with the depletion of serotonin, dopamine, norepinephrine, epinephrine, thiols (homocysteine, L-methionine, S-adenosyl-L-methionine, S-adenosyl-homocysteine, cystathione, L-cysteine, and glutathione), L-tyrosine, and L-tryptophan, and these depletions represent relative nutritional deficiencies (RNDs) where systemic nutritional synthesis requirements cannot be achieved on a normal or optimal diet…When [L-dopa is] administered singularly or with an improper nutrient balance, it has the ability to induce RNDs of serotonin, thiols, L-tyrosine, and L-tryptophan”
Leaving out that you often see high levels of plasma homocysteine in people with PD, and implying that they are low, is a troubling omission. If it’s known that L-dopa can cause increased homocysteine levels (for a reference, see https://www.ncbi.nlm.nih.gov/pubmed/20214564), why not mention that in your nutrient discussion? Why imply that it’s deficient (thiols…)? Remember the crux of the paper is that carbidopa kills you by depleting vitamin B6. A quick google search brought up something interesting: http://www.uofmhealth.org/health-library/hn-1418007… which says
“Levodopa is broken down in the body by a process requiring vitamin B6. Breakdown may deplete available vitamin B6… For people taking levodopa alone, small amounts of vitamin B6 (5–10 mg per day) may prevent levodopa-induced vitamin B6 deficiency.”
To explain this requires a bit of biochemistry. The breakdown of dopamine requires two enzymes: MAO and COMT (both PD drug targets). COMT, or catechol-O-methyltransferase, is an enzyme which moves around a single methyl group. There are only a few ways that methyl groups can get moved around… and folate is a huge player in it. The methyl group donor for this reaction is S-adenosyl methionine (SAM)… this probably means very little to you so far. But, when SAM donates a methyl group, it forms S-adenosyl homocysteine, when then goes on to form homocysteine. Now we have a link between L-dopa and homocysteine… when dopamine is broken down, you’ll make homocysteine. Now, you may ask, how do we get rid of homocysteine? Well, there are two ways. One recycles homocysteine back to methionine (which in turn can form SAM) and requires vitamin B12, folate, and multiple enzymes. The other way to get rid of homocysteine requires a different vitamin…. guess… yep, vitamin B6.
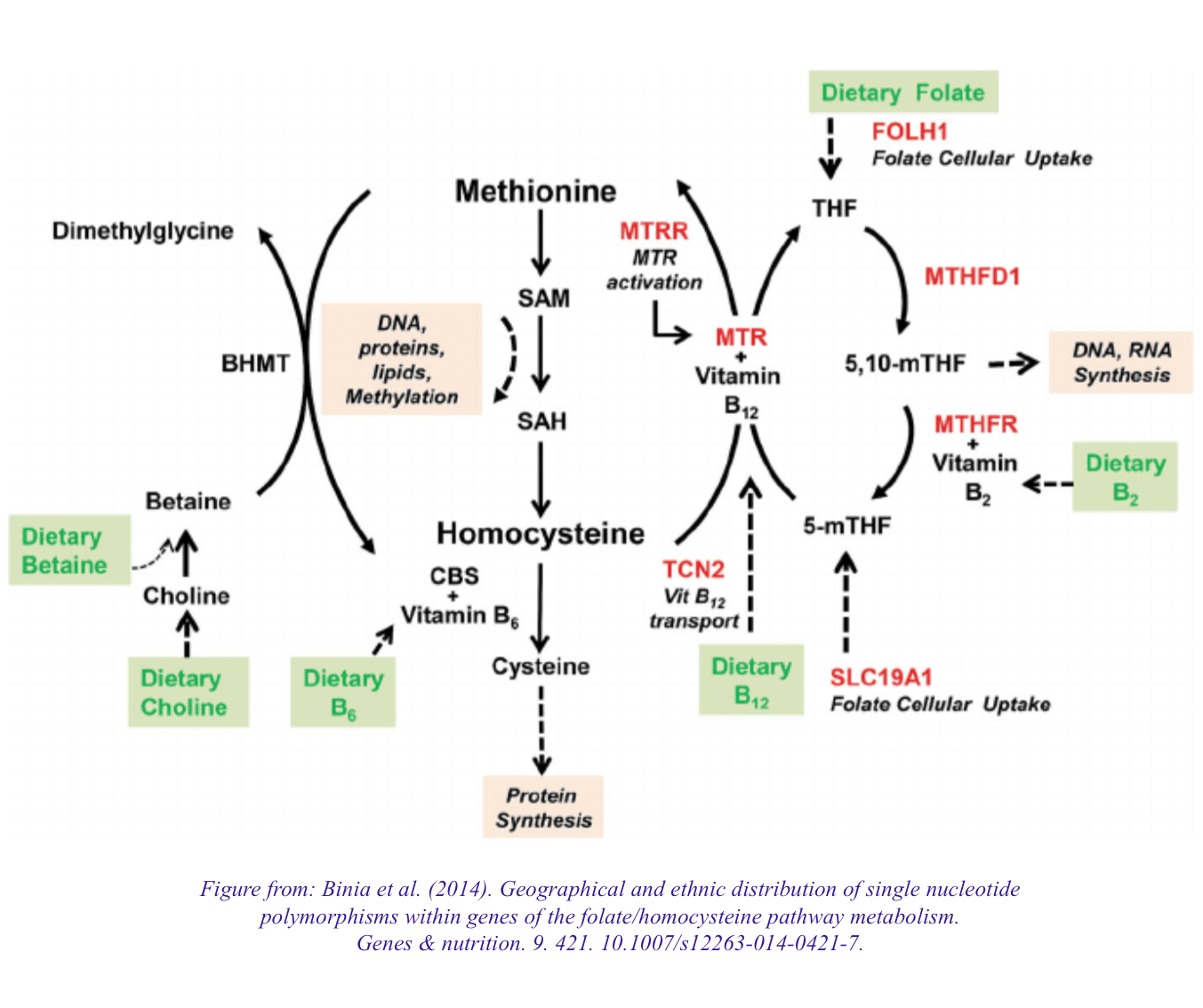
So why could taking levodopa alone cause vitamin B6 deficiency? Well, if you’re taking L-dopa without a DCC inhibitor, you need pretty high doses in order to get a reasonable amount into the central nervous system. This means you’ll be making a lot of dopamine peripherally, which will get degraded into homocysteine. To try to keep homocysteine levels down, you may use a lot of vitamin B6. Carbidopa can minimize this effect through decreasing the total amount of dopamine which is formed. Remember, patients take lower doses of L-dopa when they also take carbidopa.
So we’ve come full circle… high-dose carbidopa can reduce PLP levels (which is formed from B6), patients with PD need L-dopa, and carbidopa could help prevent B6 depletion due to administering L-dopa. What’s the take-away? The amounts matter… the relative preference of carbidopa for DCC compared to PLP and other enzymes requiring PLP matters. The dosage of carbidopa matters. But cherry picking data and insinuating that doctors are intentionally harming their patients is dubious and wrong. I think we’d like to believe that scientists and doctors are always truthful… but that’s not always the case. There are biases, there are motives, and often, there are financial incentives. Be skeptical, do your research, and ask questions. Just be sure to ask questions from people other than just the authors of a given paper.
I’m particularly skeptical when I see people publishing data to help sell expensive supplements. I have no problems with supplements, as long as they are not supplements only because they could not be approved as drugs. Remember, they are not regulated. You do not have to prove that they actually work or help. If a drug (L-dopa) is being given as a supplement… consider why. How much is it? What’s the background of the scientist/doctor? There are many drugs based on natural substances which could be sold as supplements. There’s a reason people typically don’t take foxglove as a supplement on their own… even though it’s what digoxin is made from. “Natural” is not always better when it comes to comparing supplements to drugs.
Finally, one last quote from Hinz et al.:
“Simply describing carbidopa and benserazide as decarboxylase inhibitors is analogous to describing a nuclear blast as a window breaker. Chronic administration affects virtually every system in the body.” I would like to laugh at the fact that their citation is simply a list of enzymes which PLP interacts with in humans (which may or may not be affected, again coming back to relative binding affinities and dosage)… but it scares me that people may read this and believe that they truly have data to backup a statement like that. They are overstating and overclaiming, using language to try to scare you into avoiding carbidopa at all costs. Why might this be beneficial to them? Well, if you can't buy L-dopa as a drug without carbidopa, that leaves you with products such as their supplements... costing a few hundred to a few thousand per month.
I’ll now admit… I did not put much faith into the paper being a good piece of scientific work the moment I read the first few sentences. But looking into the science confirmed my initial doubts, and hopefully some of you will find my detective work useful.
To summarize what I found:
-
The death rate chart is incredibly misleading, and there was significant data manipulation to create the graph
-
There is no convincing data indicating that carbidopa causes increased death rates
-
Vitamin B6 biochemistry is complicated, and is affected by L-dopa and carbidopa (and genetics, epigenetics, other drugs, nutrition, etc.)
-
Supplements selling “natural” L-dopa are still L-dopa… whether it’s made in a lab or a plant, it’s the same compound.
-
My husband took his carbidopa/levodopa this morning
If you would like to know more about the background of Marty Hinz, please read the following articles, which I think paint a better picture of his bias and possible goals.
https://www.casewatch.org/board/med/hinz/HINZ,%20Martin%20C%205-12-01.pdf
http://caselaw.findlaw.com/us-8th-circuit/1336355.html
http://www.startribune.com/fda-acts-against-duluth-firm-selling-dietary-supplements/129808958/
Here are also a few papers which show other possible benefits of carbidopa, if you're interested:
https://www.ncbi.nlm.nih.gov/pubmed/28898256
https://www.ncbi.nlm.nih.gov/pubmed/28963435